History of Cancer
The following text is a transcript of the podcast “Le cancer, quelles histoires” (in french only).
In recent years, the idea that cancer is a recent disease, the causes of which are linked to our modern way of life, has spread quite widely in some media and on social networks. However, as we will see in this podcast, the history of cancer is probably as old as mankind, and it might even be older than that. In this episode, we will take an incredible journey back in time over 1.7 million years. Since ancient Egypt, cancer has been studied, questioned, feared, and most of all, has killed. This journey into the great History of cancer is also a journey into the great History of medicine, and will allow us to recall the many events, changes, theories and discoveries that have marked it for millennia.
Let’s start by opening the book of the great History of cancer by going back to the first cases, suspicions of cancers found by archaeologists. In 2016, researchers from the University of Witwatersrand and the African Center for Excellence in Paleo-Sciences published a remarkable discovery in the South African Journal of Science. Near Johannesburg, South Africa, in the cave of Swartkrans, they discovered 1.7 million years old fragments of hominids. On a bone fragment of the foot, they detected a growth corresponding to osteosarcoma, an invasive tumor. On the occasion of this discovery, the late Prof. Thomas Tursz, who headed the Gustave Roussy Institute, the first European cancer research center, told the radio station France Culture the following: “The idea that cancer is a very old disease is already widely known. There is a dinosaur in Wyoming that also had osteosarcoma. […] On the skeletons, the anthropology of cancer is difficult to do since we only have bone tumors, which represent only a small part of tumors. These are either relatively rare primary tumors or metastases. […] I know that the pithecanthrope of Java […], which is only 600,000 years old, also had osteosarcoma, and that we found in Neolithic men kept in ice in Germany or Austria, tumors, also on the bones. So, the idea that cancer is a recent disease is wrong.” Besides, throughout human history, many testimonies of forms of cancer were made. Before this incredible discovery from South Africa, the oldest trace of cancer came from the Lazaret cave, near Nice, in France. A cranial bone from a young pre-Neanderthal had been found there, and the latter presented a lesion that suggested a meningioma, a brain tumor. It is estimated that these bones dated back to 150,000 years.
Let’s now take a huge step forward in time to go straight to ancient Egypt, where archaeologists found stigmata of cancer on mummies. Éric Barthelmé, in a communication presented at the meeting of June 13, 1981 of the French Society for the History of Medicine, and entitled History of the notion of cancer, explained, and I quote: “We can quote in this regard the observation reported by Granville in 1825: the dissection of a mummy of the Ptolemaic era made him discover a tumor mass including the ovary and the right parameter, associated with stigmata of ascitic effusions and an increase in volume of the uterus.” In 2015, a Spanish research team also found 4,200-year-old remains in southern Egypt with traces of cancer. The research focused on the necropolis of the Elephantine aristocracy; a very active trade hub at the time. After analysis, the research team determined that two of the people in the necropolis had suffered from cancer. The mummy of a woman notably showed traces of Kahler’s disease, a cancer developing from cells found in the bone marrow and generating blood cells. Egyptian civilization, very advanced for its time, understood what cancer could be, but as advanced as it was, had failed to put in place effective treatments. The Ebers papyrus, considered to be one of the first true medical documents, indeed referred to cancer. This document, discovered in Luxor in 1862 by Edwin Smith and bought by the German Egyptologist Georg Moritz Ebers in 1872, is the proof that the Egyptians managed to distinguish between several diseases, and in particular cancer, where reports of conditions affecting the uterus, stomach and chest were present. Against these affections, considered to be linked to the divine, the text recommends, and I quote: ” do thou nothing there against.” This papyrus, which is in fact a 110-page scroll measuring over twenty meters long by 30 centimeters wide, was probably written between 1600 and 1500 BCE, during the reign of Amenhotep I, and it would be necessary to wait nearly a millennium to find mentions of cancer much more precise in ancient Greece.
Indeed, the famous Greek historian and geographer Herodotus, who lived in the 5th century BCE, told us the story of the Persian Queen Atossa. The future regent of the Persian Empire and mother of the very famous Xerxes began to have a breast growth. She didn’t tell anyone about it first, until the growth was no longer hideable. Atossa then brought the famous Greek doctor Democedes to her. The reason for the presence of this Greek in present-day Iran is explained by its capture in 522 BCE by the Satrap of Sardis (Western Turkey). Sent as a slave to Susa, in present-day Iran, he managed to convince the Queen of the Persians to remove her tumor, which had worsened, causing bleeding and oozing. As Yolande Arnault points out in her 2017 book, Cancer, a long silent disease: “Can we just imagine under what conditions the unfortunate Atossa could have suffered such an act? What abyss of suffering did this woman face?” Our Greek doctor, Democedes, who nevertheless managed to cure the Queen, was granted as a reward the freedom to return to Greece permanently.
But how would it be possible to discuss ancient Greece and medicine without mentioning the man who is considered the “father of medicine”: Hippocrates. Indeed, the term cancer comes directly from him. He was the first to compare cancer to a crab (καρκίνος in ancient Greek) because the tumor lesion has “veins extended on all sides, just as the crab has feet.” In his writings, Hippocrates described various tumors, including the ones of the skin, rectum, breast and uterus. In order to be able to treat these affections, Hippocrates referred to the Theory of Humors, which we have already mentioned several times in the previous months. This theory suggested that the human body is made up of four substances called Humors. The latter had to maintain a perfect balance between them. When an illness arose, it meant that the balance was upset. The four humors were actually four liquids: black bile, yellow bile, lymph and blood. If the disease was pronounced, it was then necessary to carry out periodic micturition, the fact of evacuating any substance or liquid present in the body. Most of the time, the body took care of it naturally: black bile, yellow bile and lymph were expelled by excrement, sweat, tears and nasal discharge. The blood was generally expelled by bloodletting. In the case of tumors, for Hippocrates, they were linked to an excess of black bile.
As Eric Barthelmé points out, after the death of Hippocrates, medicine would experience a “long period of stagnation”, which does not mean that the study of cancer and tumors stopped. Indeed, a few centuries later, Aulus Cornelius Celsus devoted an entire chapter to cancer in his treatise De Medecina – On medicine, which, nowadays, occupies a major place in the history of medicine. As André-Julien Fabre points out in his research paper Cancer in Antiquity – the teachings of Celsus, we almost know nothing about the life of Aulus Cornelius Celsus, and we don’t even know if he was a doctor. We just know that he was a citizen of the Roman Empire and that he lived in the first century AD, in the time of Emperor Augustus. In this chapter devoted to cancer, he endeavored to describe the locations, symptoms and potential treatments. But Celsus was not able to differentiate between “true tumors and inflammatory processes” and did not make any changes to Hippocrates’ theory of Humors, which would be brought up to date by Galen.
But before talking about the other emblematic figure of classical medicine, let’s take the time to talk about Aretaeus of Cappadocia, a man about whom we know almost nothing, just like Celsus. From his name, it is possible to deduce that he was a native of central Anatolia, in present-day Turkey. He may have lived between the 1st and the 2nd century AD. Aretaeus left us a work: On the Causes, Symptoms and Cure of Acute and Chronic Diseases, which consists of eight books. In the chapter titled Uterine Disorders, he said, and I quote: “The opening of the uterus in women is suitable for menstruation and childbearing but is conducive to many serious diseases.” He is therefore making a reference to uterine cancer, and attributes it, like his contemporaries, to an excess of black bile. Aretaeus of Cappadocia however emphasized two distinct types of uterine affections, I quote: “the ulcerated one, which can be large, irritating and painful, and the non-ulcerated one, which is firm.” With regard to the ulcerated uterine carcinoma, the cancerous tumor, he made the following observation: “The purulent discharge is substantial … The lips of the ulcer are hard and rough. There is a certain amount of blood mixed with pus, very repulsive, and the pain is severe. The ulcer corrupts the uterus, and sometimes a loose, fleshy substance comes out, does not heal, and causes death. The lips of the uterus swell under the tension of the surrounding parts.” Aretaeus of Cappadocia also specified that the women suffering from this affection were in an incurable state, had fever and suffered from acute pains, making any medical application difficult. Remarkable for their precision, Aretaeus’ writings also characterize him as an accomplished observer and above all, as a doctor concerned more about his patients than theory. A point which widely differentiates it from other ancient authors.
If Aretaeus of Cappadocia focused on cancer of the uterus, another ancient physician, who was moreover very plausibly one of his contemporaries, chose to focus on breast cancer: Leonidas. Obviously, we are not talking about the legendary King of Sparta who illustrated himself with his famous “300” during the battle of Thermopylae, but a doctor from the Egyptian city of Alexandria, who was considered a great specialist in breast cancer surgery. Of his technique, we still have writings, especially of his students, like those of a certain Aetius of Amide, who explained Leonidas’ method: “I make the patient lie on her back. Then, I make an incision over the cancer on the healthy part of the breast, which I cauterize until a crust occurs indicating the stop of the blood. Then I make a new incision and dissect the breast deeply and again I burn what has been cut. I cut, I burn to avoid blood. This avoids the danger of a hemorrhage. After the amputation is completely finished, I burn all the parts again until they are dry. The first cauterizations are intended to stop the blood, the last to destroy all the evil that can remain.” This description of Leonidas’ method inspired breast surgery for many centuries and gives us an extremely detailed overview of the methods of the time. It is then difficult not to think of Queen Atossa of Persia and not to adapt the formula used by Yolande Arnault to describe the sufferings of the Queen, to all these women who for centuries and centuries have gone through this surgical procedure without anesthesia: “Can we just imagine what abysses of suffering these women have faced.”
Regarding the causes of these cancers, the general belief at that time was therefore linked to the theory of Humors, a theory which was reconfirmed by Claudius Galenus, also known as Galen. Aglançon, the master of Galen, was however the first to revise this theory, as Éric Barthelmé explains: “According to the new formulation, the liver produces black bile instead of blood when the temperature rises. As the spleen is unable to absorb excess atrabile (black bile), the blood thickens, becomes cloudy, and its stagnation in any organ leads to the development of neoplastic disease.” Galen, who was with Hippocrates one of the two greatest theoreticians of ancient medicine, explained that the tumor was the “direct consequence” of an excess of black bile. He was the most famous doctor of his time and cared for several emperors. Originally from the radiant city of Pergamon, in present-day Turkey, he travelled in the Greco-Roman world after the death of his father, the year of his 19th birthday. From 169 to 193 AD, he was responsible, among other things, for the health of the Roman Emperors Marcus Aurelius and Commodus. It is to Galen that we owe the word sarcoma, designating soft tissue tumours, which he individualized for the first time. It is also to him that we owe the word oncology, since he used the Greek word oncos (ὄγκος) to designate a growth, or probably a malignant tumor.
As you may have noticed, a number of these prestigious thinkers and physicians of the Antiquity were from Anatolia, passed through the Persian Empire or lived, studied in or visited Egypt. You will therefore not be surprised to know that the progresses that followed came from the Arab world. But these progresses would not follow until quite late. On the one hand, because the fall of the Roman Empire in the West no longer constituted a favorable environment for the advancement of science, and on the other hand because this fall also led to the loss of certain knowledge. Many books, treatises and essays had indeed not been translated from Greek into Latin, and the Christian world which was emerging in Western Europe after the fall of the Empire in 476, did not give priority to the translation of these writings. This translation enterprise, which hid above all a thirst for knowledge and discovery, was finally set in motion by the Arab peoples. And it is thanks to them in particular that modern concepts of cancerology came to us. Let’s therefore head to Baghdad, at the very beginning of the 11th century, where a philosopher and doctor named Avicenna became very interested in cancer. He described the slow progression of the cancer, invading and destroying adjacent tissues. We owe in particular to Avicenna his Books of medical laws, composed of five volumes, which were brought by Europeans in the West and which influenced the practice of medicine in Europe until the new ideas of the Renaissance. History has not forgotten Avicenna, as evidenced by the many medical establishments that still bear his name today.
Shortly after him, but this time on the side of Muslim Spain, and more specifically in Cordoba, the next comments on cancer came from a doctor named Abulcasis. Albucasis did in fact use the principles advanced by Leonidas, almost a thousand years before him, while adding a few clarifications. Cordoba’s doctor recommended ablation when the cancer was still in its early stage, and, like Leonidas, recommended cauterizing adjacent tissue. With regard to tumors already in advanced stages, Albucasis was lucid enough to prevent any form of treatment, which he deemed ineffective in the face of the disease and would thus save many of its patients from an unnecessary suffering. A few years later, in the first half of the 12th century, Avenzoar, also a doctor in Cordoba, was the first to describe esophageal cancer. Very famous during his lifetime, since he was nicknamed the “famous wise man” by his contemporaries, Avenzoar had for disciple Averroes, one of the most influential thinkers of the Middle Ages. Ironically, our famous wise man died from a tumor, which he himself tried to cure and whose inevitable progress he noted. Arab medicine would continue to influence medicine for a few centuries, including in Western Europe, before being called into question, as well as the theory of Humors and the teachings of Hippocrates and Galen, by Renaissance scientists.
A major fact allowed lasting progresses: the authorization of the autopsy by the Catholic Church. Even in Rome, before the beginnings of Christianity, the human body was described as inviolable. Galen himself did not perform an autopsy, or otherwise very informally, and had to content himself with dissecting animals, and more particularly monkeys. With the advent of Christianity in Europe at the end of antiquity and during the Middle Ages, the inviolability of the human body remained the law, and those who chose to perform autopsies took tremendous risks. In 1300, in his Decretum of Sepultaris, Pope Boniface VIII announced systematic excommunication to all those who, and I quote: “would extract the viscera from the bodies of the deceased to make a horrible and detestable abuse.” Over the centuries and decades, however, autopsies were gradually accepted, first in exceptional cases, such as during the epidemic of black plague which struck Europe violently in the 14th century, before being widely tolerated from the first half of the 16th century. Anatomical knowledge then developed rapidly and made it possible to discredit many theories which had hitherto influenced the practice of medicine.
And it was in this context that Andreas Vesalius, a brilliant anatomist born in Brussels, at the time located in the Duchy of Brabant, under the domination of the Holy German Empire, intervened. In his treatise De humani corporis fabrica – On the fabric of human body, he refuted ancient theories, sweeping away any link between health and Humors. This document consisted of 700 pages, with hundreds of extremely precise drawings on the human body. One of Vesalius’ main assumptions was that the human body should be thoroughly inspected before being described. Nearly 1,400 years after Galen, the existence of black bile was finally disproved thanks to his work, even though many principles of the Theory of Humours continued to wrongly influence the medical field. The old ideas and beliefs, even if proven false, were indeed hard-skinned, for Molière would still make fun of them in The Imaginary Invalid in 1673, more than a hundred years after the death of Vesalius. Vesalius ended up teaching at the prestigious University of Padua, in Italy, and is today considered the greatest anatomist of the Renaissance.
One of Vesalius’ students at the University of Padua, Gabriele Fallopius, completed and corrected the work of his master. In his Historical Dictionary of Ancient and Modern Medicine, published in 1778, Nicolas Eloy, a French physician, said about Fallopius: “He corrected very well the errors that had escaped Vesalius […] but as he was not of a presumptuous character, he proposes his discoveries with modesty, and fights the errors of others with moderation. All his life he had the utmost respect for Vesalius, his master, and he never violated the rights of friendship towards anyone.” But more than correcting Vesalius’ little mistakes, Fallopius also described the clinical differences between malignant and benign tumors as we know them today. I quote Mohammed Hamyeh, who in his doctoral dissertation on the regulation by a protein of a mammary tumor aggressiveness, defended in 2016, gave us details on the discoveries of our 16th century Italian doctor: “He characterized malignant tumors by their ligneous firmness, irregular shapes, multi-lobulation, adhesion to surrounding tissues and by congested blood vessels around the lesion.” At that time, most of the progress came from Italy. For most of the Renaissance, the peninsula was the artistic, cultural and scientific center of Europe.
And so, logically, shortly after Fallopius, it was another Italian, Gaspard Aselli, who was at the origin of a new great discovery. Aselli was indeed the first to discover the basics of lymphatic functioning at the start of the 17th century, whose role is decisive in the spread of cancer. It should also be noted that this discovery by Aselli coincides with another great discovery by one of his contemporaries: that of blood circulation by William Harvey. And these two major discoveries further challenged humoral medicine. Still around the same time, but on Naples’ side, Professor of anatomy and surgery Marco Aurelio Severino published in 1632 De recondita abscessuum natura – The hidden nature of abscesses where he described the different tumors linked to breast cancer, distinguishing benign from malignant. He also recommended removing benign tumors to prevent them from getting worse, and stood out by adding illustrations in his treatises, like Vesalius. Also, at this time, that is to say at the beginning of the XVIIth century, it was in Germany that a “method of curing cancer” was born, as described in the Complete Treatise on Surgical Operations, published in 1698. And this method was the fact of Wilhelm Fabricius Hildanus, considered today as the father of German surgery. He was the first to use tourniquets to control bleeding and introduced the concept of removing enlarged lymph nodes in breast cancer operations.
The history of cancer was then deeply marked by the work of Jean Pecquet, a French doctor who lived in the heart of the 17th century (1622-1674). Pecquet is responsible for the discovery of the thoracic duct, the main collector of the lymphatic vessels which had been discovered a century earlier by Fallopius. Here is how the Larousse describes and explains this important discovery: “Pecquet, by experimenting on the dog, discovered in 1647 that all the lymphatic vessels of the intestine […], very visible during the digestive periods, converge towards a reservoir located in front of the lumbar spine, the Pecquet cistern, and that this gives birth to the thoracic duct, which brings the lymph back to the heart.” It would take a long time before scientists realize the importance of this discovery in the evolution of cancer and its treatment, the lymphatic system playing a major role in the course of the disease.
Throughout history, many diseases were often misunderstood, and people with cancer have suffered the consequences of these biases over the centuries. One of the big questions about cancer was whether it was contagious. It is possible to cite, in this case, the conclusions of Daniel Stennert, a German doctor who lived over the XVIth and XVIIth centuries, to whom we notably attributed the first clinical description of Rubella, in 1619. According to some sources, he was the one of those who participated in the idea that cancer was a contagious disease. James Stuart Olson, in The History of Cancer: An Annotated Bibliography, explains this to us: “Daniel Stennert concludes that cancer was contagious and helped initiate feelings of shame, horror, and the brand of infamy that has since been associated with it.” This feeling impacted the care of the sick for many years, to the point that some doctors of the time rebelled against this injustice. This is particularly the case of Jean Godinot, who was canon of the Cathedral of Reims. Very touched by the situation of these patients rejected by the population, he proposed an endowment for the foundation of a hospital for cancer patients. A proposal which was accepted on August 25, 1740, up to 25,000 pounds (approximately 300,000 euros today). Thus, the website of the Godinot Institute in Reims, France, dedicated today to cancer research, care and education, specifies: “Was founded more than two centuries before the time, the world’s first cancer center.”
Going back to the Theory of Humors, and as we saw in this discussion, there was no shortage of scientific evidence challenging this theory during the Renaissance. In the second part of the Modern era, humoral medicine still strongly influenced practices. A French doctor, however, helped discrediting this theory a little bit more: Henri François Le Dran, chief surgeon at the Charité hospital in Paris and surgeon to the king. Le Dran was one of the first surgeons to specialize in the treatment of cancer. He published in 1742 his Treatise on surgical operations where he developed his theory on the treatment of cancer, which was similar to some of its predecessors. His premise was that the cancer begins in a specific place, and then gradually spreads through the lymphatic channels to the lymph nodes, which would explain why, for example, breast cancer can reach the lungs. Regarding treatment, he advocated excision of the tumor and lymph nodes, understanding that from the moment the lymph nodes were affected, the disease was serious.
Nearly fifty years later and still in France, Marie François-Xavier Bichat, a brilliant young doctor, worked among other things on the different localizations of cancer, thus completing Le Dran’s work by proving that these different affected places are in fact from the same disease, and clarifies the concept of distant metastasis. Unfortunately for the progress of medicine at that time, this brilliant scientist died prematurely of typhoid fever at the age of thirty years old. However, he is today considered the father of modern histology: the study of biological tissue. In his work Physiological Research on Life and Death published in 1800, he said, and I quote: “Life is the set of functions that resist death.” Unfortunately, at the time of Bichat, cancer was still far too strong for human science.
Let’s leave France and go back in time, to the University of Padua, in Italy, where anatomical pathology was born, which according to the French National Cancer Institute is, and I quote: “the medical specialty which consists in examining organs, tissues or cells to find and analyze abnormalities related to a disease.” It was Giovanni Battista Morgagni who was behind its advent. In 1761, this Italian doctor published De Sedibus and Causis Morburum – Of the seats and causes of diseases investigated through anatomy, which reports on almost 60 years of work. Morgagni was indeed 79 years old when his work was published. This gave him the time to perform more than 700 autopsies. In an epistolary style characteristic of the time, he listed cases of breast, stomach, pancreas and rectum cancer, thus constituting the first coherent treatise on anatomical pathology, since his dissections were carried out in the purpose of knowing the lesions that caused the subject’s death.
The beginnings of this medical specialty preceded an astonishing discovery for the time. In 1775, Percival Pott, a British surgeon, described the first case of “occupational cancer”: chimney sweep carcinoma. In his book Chirurgical Observations, he sweeps away the preconceived idea that this affection was a venereal disease, because of its localization, since it touched the scrotum. For Pott, this cancer was due to the soot and tar that permeated the clothes and the folds of skin covering the testicles of chimney sweeps. Here is how, according to his words, Percival Pott described the chimney sweeper’s cancer: ” It is a disease which always makes it first attack on the inferior part of the scrotum where it produces a superficial, painful ragged ill-looking sore with hard rising edges…..in no great length of time it pervades the skin, dartos and the membranes of the scrotum, and seizes the testicle, which it enlarges, hardens and renders truly and thoroughly distempered. Whence it makes its way up the spermatic process into the abdomen.” He was thus the first to put forward the hypothesis that a malignant tumor may be due to a carcinogenic environment, and therefore contributed to making epidemiology a true science. Percival Pott was the most eminent surgeon in his country and was notably elected Master of the Company of Surgeons, the forerunner of the Royal College of Surgeons, in 1765. He used his reputation to improve the working conditions of chimney sweeps, and especially children, since it must be remembered that many children were working at the time, sometimes as young as four years old. In 1788, the Chimney Sweeper’s Act was promulgated. This act stipulated that no boy should be apprenticed before being eight years old. Parents’ consent had to be obtained, and the master chimney sweep had to promise to provide suitable clothing and living conditions, as well as the possibility of going to church on Sunday. A small victory that Pott was able to savor before dying the same year, at the age of 74.
Pott’s influence didn’t stop there, as his student, John Hunter, also made remarkable contributions to the great history of cancer. In The Complete Works of John Hunter, a collection of all his publications, he made many remarks on the disease, and put forward in particular an innovative theory: is cancer hereditary? To this question, he specifies: “There are doctors who believe that cancer is hereditary, but all that I can admit according to my principles on the inheritance of diseases, is that the subjects from parents who had a strong disposition or susceptibility for a particular disease, may also have the same disposition or susceptibility.” He also established three main causes of the disease: a particular organ, age, and the state of that particular organ at that age. According to Hunter, the average age to develop cancer is between 40 and 60 years old.
The next generation was marked by René-Théophile Laennec. Laennec is today mainly known for having created the stethoscope, which allowed him to become the creator of medical diagnostic by auscultation. Regarding cancer, Laennec had a real understanding of the disease very early on, describing various tumors and their evolution. He was notably at the origin of the word melanoma. In 1804, while still a student, he was already lecturing on this subject. Laennec was in fact the first to admit that the melanotic lesions were metastatic and not black tuberculous granulomas or the carbon deposits frequently found in the lungs during the autopsy. To invent the term melanoma, he was inspired by the ancient Greek, where melas (μέλας) meant black. Considered as a central figure in the history of medicine, Laennec is also known and recognized for his extreme scientific rigor. In 1819, he published De auscultation mediate – A treatise on the diagnosis of diseases of the lungs and heart, based mainly on this new means of exploration. Held in high esteem by his contemporaries and the following generations, this two-volume treaty allowed Laennec to enter another dimension. Benjamin Ward Richardson (1828-1896), an English physician who created the Journal of Public Health and Sanitory Review, declared in his book Disciples of Aesculapius: “the true medical student must read Laennec’s treatise on mediated auscultation and the use of the stethoscope at least once every two years, as long as he practices his art. His original work places him among the great pioneers alongside Vesalius, Harvey and Hippocrates.”
Shortly after Laennec’s death in 1826, the German Johannes Peter Muller continued the cycle of progresses linked to the understanding of what cancer is. Muller was indeed one of the first to use the microscope to develop his theories and therefore dove into promising research. From 1833 to 1840, he published Handbuch der physiologie des Menschen – Manual of human physiology, his magnum opus, where, for the first time in the history of medicine, he combined knowledge from chemistry and physics with human anatomy. Thanks to the work of his assistant, Theodor Schwann, who succeeded in showing that cells are the basic unit of the structure of the animal world, Muller was able to focus on the cellular structure of tumors, using the famous microscope. As you can see by now, the general belief at the time was that cancer was a general disease, and that the tumor was a local manifestation. In this context, Muller was the first to assert that cancer is linked to an increase in abnormal cells. To better understand Muller’s work, I quote Eric Schirman and José de la Heras, who in their book Cancer Biology and the Nuclear Envelope – Recent Advances May Elucidate Past Paradoxes, explained these principles: “In On the nature and structural characteristics of cancer and these morbid growths that may be co-founded, [Muller] was the first to describe cancer cells in detail and note how they lose their adhesion to normal cells. Based on the physical characteristics he observed, such as altered cell morphology, cell adhesion is reduced and the rigidity of the tumor mass altered relative to the surrounding tissue, Muller developed criteria for diagnosing benign and malignant, as well as to distinguish sarcomas (tumors with abundant tissue connectivity) from carcinomas (tumors with little or no connective tissue).” This work, dating from 1838, had a preponderant influence on his peers and on the continuation of work on cancer.
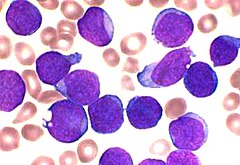
This was evidenced by the work of Rudolf Virchow, who was strongly inspired by his work and that of his assistant, Theodor Schwann. Virchow, a physician, and also a politician, is today considered as one of the founders of modern anatomical-pathology, a field that, remember, was born two hundred years earlier thanks to the work of Giovanni Morgagni Baptist. In his book entitled Zellular pathology – Cellular Pathology, published in 1858, Virchow was the first to advance the conception of cancer as purely cellular. On the concept of heredity, however, he preferred to bring a nuance, emphasizing that of favorable ground, declaring, and I quote, “It is the predisposition, not the disease, that we inherit.” Extremely versatile and multifaceted, Rudolf Virchow became a Member of the Berlin Reichstag from 1880 to 1883, worked on public hygiene, addressed issues from various fields such as archeology, anthropology, ethnology and the social issues of his time. In 1845, he had already noted the reverse balance of white and red blood cells of a disease which he would name two years later, in 1847, leukemia.
The next advances came a few decades later, at the end of the 19th century, and once again, it was a German scientist who was the originator: William Conrad Roentgen. Director of the Institute of Physics in Würzburg, he published an article in 1895 entitled About a new kind of ray in which he reported two discoveries: X-ray and radiology. Roentgen himself explained the fortunate mechanisms of his discovery in an edition of the Clune Magazine, published on April 6, 1896: “I had long been interested in cathode ray, which had been specially studied by Hertz and Lenard. [I] promised myself, as soon as I had time, to do some personal work … I found time for this at the end of October 1895. […] I was working [November 8, 1895 in the evening] with a Hittorf-Crookes tube, which was entirely surrounded by black paper. A piece of barium platinum paper sat next to it on the table. I sent a current through the tube and noticed, through the paper, a particular black line. It was excluded that light could come from the tube because it was completely covered with paper, and the paper did not let in any light … I thought … it was … something new, but still unknown.” He then realized that if you put your hand between the tube and the screen, the bones of the hand appear. Stunned by his discovery, he then called his wife to show him the results and, on the same occasion, made the very first X-ray. For this discovery, Roentgen was awarded the first ever Nobel Prize in Physics, in 1901. The X-ray would quickly leave physics laboratories to revolutionize cancer medicine and treatment.
But to cite this one discovery without citing the works of Henri Becquerel and Pierre and Marie Curie would only be telling a very incomplete story. Indeed, the discovery of Roentgen called to mind Henri Becquerel, a French physicist. Becquerel began to work on this subject and eventually “discovered” what was called shortly after radioactivity, by demonstrating that uranium salts emit rays different from X-rays. He then named them uranium rays. Around the same time, Marie Curie, then aged 29, was looking for a subject to write her PhD. Roentgen’s discovery had caused a lot of talk in the scientific community, but that of Becquerel had remained much more confidential. The perfect opportunity to work on a subject more than promising for Marie Curie, who began working on the project in 1897. More particularly, she studied the radiation produced by uranium, and quickly deduced that the intensity of the radiation is proportional to the quantity of uranium and, shortly after, that this radiation is an atomic property, specific to the atom. She called this phenomenon radioactivity. Then followed a period of four years of work with her husband Pierre Curie, composed, among other things, of the discovery of radium, the study of radioactivity and many published articles. This work earned the Curie couple, as well as Henri Becquerel, the Nobel Prize in Physics in 1903. The radioactivity of radium sparked enthusiasm and it was soon realized that this chemical element could have medical virtues. Very quickly, medical personnel began to use needles and other radium applicators to try to treat tumors and skin cancers.
In 1901, Henri Dalos, a dermatologist working at the Saint Louis hospital in Paris, borrowed a few milligrams of radium from Pierre Curie and experimented for the first time on human tumors. The results were promising, and radium would soon become the basis of fashionable products from industry, pharmacology and everyday life: soap, toilet water and all kinds of medicines. And it was only much later that the general public would realize the harmful effects of radium on health, leading to the creation of a legal framework, which started to limit its use in the 1920s. In 1934, the French Ministry of Labour classified as occupational diseases the ones resulting from the manufacture of radium salts, and three years later, in 1937, this chemical element was prohibited except in the field of medicine, where its use was henceforth very restricted. Let’s also note that radium was permanently abandoned by the medical field in 1976 and was replaced by Iridium-192 and Cesium-137 in radiotherapy, for reasons of radiation protection, which aims to prevent or reduce the risks linked to ionizing radiation.
As in all areas that we have studied in recent months, the end of the 19th and the beginning of the 20th century marked a turning point in the history of medicine. Progress then followed at an exponential speed. However, at the beginning of the 20th century, it was only possible to treat by surgery or radiotherapy localized cancers. In 1911, German immunologist August van Wassermann tested selenium, a chemical, on a mouse sarcoma, and achieved perfect remission. Unfortunately, von Wassermann soon realized that the cytotoxicity of selenium – that is, its toxic effect on cells – was far too important to consider treating humans. On the French side, the League against Cancer was created on March 14, 1918, and was recognized as an association of public utility in November 1920.
We understood, especially with the works of Percival Pott at the end of the 18th century, that the industrial era allowed an incredible development of the society, unfortunately often at the cost of the health of the workers, who often faced extreme, even inhuman, working conditions. These workers were exposed to very dangerous substances and elements over the decades. It is in this context that two Japanese doctors, a teacher and his student, started working on carcinogens. In 1915, Katsusaburo Yamagiwa, the master, and Koichi Ichikawa, the pupil, were the first to successfully reproduce carcinogenesis in a controlled laboratory. In their laboratory at the University of Tokyo, they reported that the repeated application of tar on the ears of rabbits led to the appearance of carcinoma, making this substance a carcinogen. On the occasion of this discovery, Yamagiwa wrote a haiku – a very short Japanese poem celebrating the evanescence of things, I quote:
Cancer has been produced, I proudly walk a few steps.
As radiation therapy grew rapidly, another area of science was starting to get a lot of talk. This was our topic for the month of December: genetics, which as a reminder refers to the study of the transmission of hereditary traits and the function of genes. One of its most prominent contributors was Theodor Boveri, a German biologist. He worked in particular on the concepts of cancer. And in 1902, he was the first to put forward the idea that cancer is a cell disease, stating that the origin of a tumor comes from the uncontrolled division of a cell. A theory which was widely rejected by his contemporaries, but which was later confirmed. I quote Professor Alain Puisieux, Director of the Cancer Research Center of Lyon, who said to the Institut Curie website on this subject: “The deregulation of a single cell is the cause of cancer. It is most often a mutation in a gene that controls its division. The cell then multiplies uncontrollably. But to lead to the development of a tumor, new cells must acquire other genetic abnormalities regarding their survival or their ability to ignore regulatory signals from their environment. Five to ten different genetic events are usually necessary to give birth to cancer.”
As the scientific community began to understand more and more the origin and development of cancer, its treatment, at the same time, was also being developed. As you may have already understood, we are going to talk about the beginnings of chemotherapy. And what’s amazing to us is that its beginnings were not necessarily linked to cancer, but to syphilis, a sexually transmitted and highly contagious infection. To be more precise, let us return to the meaning of the term chemotherapy. I quote François Chat, Professor of Pharmacy: “Until the end of the XIXth century, the whole pharmacy was dominated by the vegetable kingdom. Plants were used to cure illnesses. Starting with Paul Ehrlich and Paul Ehrlich’s pupils, we gradually introduced therapeutically substances prepared by human hands into synthetic laboratories. This is chemotherapy, these are drugs of chemical origin.” So, who is Paul Ehrlich and what has he managed to achieve? In 1909, this German doctor, chemist and physiologist managed to develop a derivative of arsenic, less toxic, and very effective against syphilis, which was still an incurable disease at the time. Arsphenamine, the first synthetic drug was born and was marketed under the name of Salavaran. Unfortunately for Ehrlich, the toxicity of this arsenic derivative turned out to be too high, and the production of arsphenamine was abandoned a few years later, which does not in any way take away the title of “father of chemotherapy” from our scientist German, since it is indeed he who is at the origin of the first chemotherapeutic agent.
The era of chemotherapy was therefore launched but would not be effective until the 1940s. Éric Franconnet, in an article entitled A brief history of chemotherapy, describes it as a “fantastic puzzle of molecules to create or combine, which would experience considerable growth until today.” The new advances which followed those of Ehrlich took their origin in an unknown fact of the Second World War: the bombardment of Bari by the Luftwaffe, the Nazi military aviation, on December 2, 1943. This attack mainly aimed at the port of the city, essential for the continuation of the conquest of the Italian peninsula by the Allied forces. Bari is in the southeast of the peninsula on the Adriatic coast and was taken in September 1943 from the Axis forces. As noted, the purpose of the operation was to neutralize, for a period of time, the supplies of the Allied troops who were moving inexorably north. 17 ships were sunk, and many others were seriously damaged, including the ship SS John Harvey, which transported a very large quantity of mustard gas, the famous gas used during the trench wars of the First World War. The explosion of several barrels containing this gas then strongly contaminated the water and air in the port. The soldiers present on the spot were very affected by the gas and an abnormal fall in the white blood cells in the latter was noted in most cases. In this context, the United States Department of Defense commissioned two pharmacologists from the prestigious American University of Yale. They were Alfred Gilman and Louis Goldman. Faced with the symptoms, Gilman and Goldman were struck by an idea. Why not try to use certain mustard gas agents to try to stem the inevitable and chaotic proliferation of white blood cells, typical of leukemias? Our two American scientists then began a whole series of experiments on mice, which quickly proved conclusive. In 1946, a gas derived from mustard was injected intravenously to try to treat non-Hodgkin’s lymphoma. The operation was initially successful, but the patient’s bone marrow deteriorated rapidly thereafter. The idea of mustard gas then revealed its limits with the patient’s death in 1948.
But this failure had the merit of arousing the curiosity of the scientific world and paved the way for Sidney Farber, an American pathologist considered today as the father of modern chemotherapy. At the time of the Gilman and Goldman experiments, Farber was already working on cancer and more specifically childhood leukemia at Harvard University. And it is to him that we owe the first real cancer chemotherapy. In the early 1950s, he focused on folic acid, a vitamin that plays a key role in DNA metabolism. Studies of American soldiers who fought in the Pacific during World War II had shown that folic acid and vitamin B12 could cure pernicious and tropical anemia. Farber was convinced that a similar solution could be found to treat leukemia. He noted in particular that folic acid helps stimulate the growth and maturation of bone marrow. He then believed that a drug that can chemically block folic acid and at the same time the growth of leukemia cells, could stop the abnormal production of bone marrow linked to leukemia. And he was right! His tests were positive: remissions were seen in children with acute lymphoblastic leukemia (blood cancer that affects lymphocytes). Even though the process was still in its infancy, the results were extremely promising, and chemotherapy was, from that point, widely used. From Farber, who died in 1973, we remember this great discovery, but also his incredible devotion to his field. David G. Nathan, who chaired the Dana-Farber Cancer Institute as President, said about Farber, and I quote: “Sidney Farber was devoted to this cause, obsessed with it. Decided by the inevitable and rapid death of childhood leukemia and grieved by the reluctance of the scientific community to invest resources in the treatment of a disease that was fatal, he and his team of clinicians and laboratory scientists developed drugs that have caused temporary leukemia remedies in many children.” From the 1950s, Farber became a star consultant to the United States Congress, seeking to raise funds for cancer research. Considered a convincing speaker, his brother, Darwin Farber, said that he was a medical diplomat in a way and that, I quote: “he understood that if cancer was going to be overcome, it would require a concerted national effort and a major financial commitment of the congress.” And in 1971, the efforts of Farber and other figures in medicine finally paid off. What is now called the War on Cancer began with the signing by the President of the United States Richard Nixon of the National Cancer Act, which announced a national effort to find a remedy for cancer by providing significant funds to improve our biological understanding of the disease and develop more effective treatments.
To conclude, let us note that Farber also referred to the 1st international conference for the study of cancer, held in Germany in 1906, which had called this disease “the scourge of humanity”. Today, even if it is better understood, cancer still raises many fears. It is indeed a devious enemy capable of advancing in the shadows for several years, and being able to touch anyone, anytime. Cancer cases have multiplied in recent decades. The increase in life expectancy can explain this phenomenon, but many factors can also explain it: heavy alcohol consumption, smoking, excessive tanning, junk food, lack of physical activity and intense stress are all bad habits that can lead to cancer. The World Health Organization (WHO) also tells us that 40% of cancers are potentially preventable, 40% can be treated and 20% are treated for palliative purposes. Ten years ago, the International Union Against Cancer (IUAC) organized a global campaign to promote healthy habits in children and reduce the risk of cancer in adulthood. A campaign supported by the WHO. Each year, on the initiative of these two organizations, World Cancer Day is celebrated on February 4. In France, according to the League against Cancer, cancers represent the leading cause of death in men and the second in women. In 2018, 382 000 new cases were diagnosed in France, and 157 000 deaths were confirmed, making cancer, well and truly, and for some time, the scourge of humanity.
Sources
http://www.arcagy.org/infocancer/en-savoir-plus/cancer/le-cancer-travers-les-ages.html/http://www.centre-paul-strauss.fr/comprendre-le-cancer/histoire-et-definition
https://www.ligue-cancer.net/article/26009_le-cancer-travers-les-siecles
https://www.verywellhealth.com/the-history-of-cancer-514101
cancer.org/acs/groups/cid/documents/webcontent/002048-pdf.pdf
https://www.cancer.org/cancer/cancerbasics/thehistoryofcancer/index.html
https://cancer.about.com/od/historyofcancer/a/cancerhistory.htm
https://www.rare-cancer.org/history-of-cancer.php
https://www.biusante.parisdescartes.fr/sfhm/hsm/HSMx1981x015x002/HSMx1981x015x002x0167.pdf
https://www.hominides.com/html/actualites/cancer-tumeur-1700000-ans-hominide-1057.php
https://books.google.fr/books?id=hgx0sJvphNkC&pg=PA464&dq=Atossa+cancer&hl=fr&sa=X&ei=VdstU_3mBevP0AXQyIDYCg&ved=0CDgQ6AEwAQ#v=onepage&q=Atossa%20cancer&f=false
https://remacle.org/bloodwolf/erudits/paulegine/chirurgie.htm
https://www.biusante.parisdescartes.fr/sfhm/hsm/HSMx2008x042x001/HSMx2008x042x001x0063.pdf
The first accurate description of uterine carcinoma by Aretaeus of Cappadocia
https://books.google.fr/books?id=JR9xdzsRL9sC&pg=PA117&lpg=PA117&dq=leonidas+cancer+du+sein&source=bl&ots=HFgHRgYbOR&sig=ACfU3U3kSUFYP1PkiCHiuWrvHlfbZV9ELQ&hl=fr&sa=X&ved=2ahUKEwiXnqmxpZzmAhWy3eAKHcYpA1cQ6AEwAXoECAkQAQ#v=onepage&q&f=false
https://books.google.fr/books?id=iR2lAgAAQBAJ&pg=PT210&lpg=PT210&dq=avicenne+cancer+bagdad&source=bl&ots=bL0ReWAn8A&sig=ACfU3U05IGmTofPB3f112vOMWO3LHEXC7Q&hl=fr&sa=X&ved=2ahUKEwi3xYH-rqvmAhWkAmMBHUt5C0sQ6AEwBXoECAoQAQ#v=onepage&q&f=false
http://microbiologie.univ-tours.fr/virus_et_cancer.pdf
https://www.futura-sciences.com/sante/questions-reponses/cancer-cancer-oesophage-detail-1154/
https://archive.org/stream/avenzoarsavieets00coliuoft/avenzoarsavieets00coliuoft_djvu.txt
https://www.cairn.info/revue-etudes-sur-la-mort-2004-1-page-97.htm#no7
https://tel.archives-ouvertes.fr/tel-01490435/document
F.J. Eloy, Dictionnaire historique de la médecine ancienne et moderne, t. 2, 1778
https://www.revmed.ch/RMS/2015/RMS-N-460/Pathologies-vasculaires-lymphatiques-apport-de-la-lympho-fluoroscopie
https://www.aktl.org/wp/wp-content/uploads/2016/02/La-d%C3%A9couverte-du-syt%C3%A8me-lymphatique-JC-Ferrandez.pdf
https://books.google.fr/books?id=rmcw52DmOIcC&pg=PA85&lpg=PA85&dq=Fabricius+Hildanus+cancer&source=bl&ots=UvuLgfQbvB&sig=ACfU3U1vPzCK36X_7Q2V1YCJONLPTfkx1g&hl=fr&sa=X&ved=2ahUKEwjz8IqL-a3mAhWB2-AKHSc5AFcQ6AEwEHoECAgQAQ#v=onepage&q=Fabricius%20Hildanus%20cancer&f=false
https://books.google.fr/books?id=NxhmAAAAcAAJ&pg=PP26&lpg=PP26&dq=Fabricius+Hildanus+cancer&source=bl&ots=98R6wmiZRj&sig=ACfU3U2Zu8WFXvTyxjlnnSEGH0FjZSkaEQ&hl=fr&sa=X&ved=2ahUKEwjfhJ-rgq7mAhVOcBQKHREOBpcQ6AEwEnoECAgQAQ#v=onepage&q=Fabricius%20Hildanus%20cancer&f=false
https://books.google.fr/books?id=LteAUrJQyfEC&pg=PA79&lpg=PA79&dq=Fabricius+Hildanus+cancer&source=bl&ots=RMZjIGQ7Mt&sig=ACfU3U0c9gOS85cNndJTc-GKUr7YoQEU9w&hl=fr&sa=X&ved=2ahUKEwjfhJ-rgq7mAhVOcBQKHREOBpcQ6AEwEXoECAoQAQ#v=onepage&q=Fabricius%20Hildanus%20cancer&f=false
https://www.larousse.fr/archives/grande-encyclopedie/page/8308
https://books.google.fr/books?id=oAX8jOJ9uO0C&pg=PA8&lpg=PA8&dq=daniel+sennert+cancer&source=bl&ots=0XtgNcsBmY&sig=ACfU3U3x7pmP3YyEm8zWxFhFMHpoNNd6aA&hl=fr&sa=X&ved=2ahUKEwjOx5vX36_mAhWQxoUKHe3HCTQQ6AEwGnoECAoQAQ#v=onepage&q=daniel%20sennert&f=false
https://www.institutgodinot.fr/fr/l-institut/histoire/
http://www.medarus.org/Medecins/MedecinsTextes/pott_percival.htm
https://www.e-cancer.fr/Dictionnaire/A/anatomopathologie
http://www.medarus.org/Medecins/MedecinsTextes/bichat.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2413782/?page=2
https://books.google.fr/books?id=66OocI0uotwC&pg=PA692&lpg=PA692&dq=john+hunter+cancer+heredit%C3%A9&source=bl&ots=gA9Pu2hD6S&sig=ACfU3U0SpoJm4FOPWWaoFO3DuNmPiYBCoQ&hl=fr&sa=X&ved=2ahUKEwjZu9nztLDmAhVuA2MBHfaVD4kQ6AEwBHoECAkQAQ#v=onepage&q=john%20hunter%20cancer%20heredit%C3%A9&f=false
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1570491/
https://gallica.bnf.fr/blog/12022016/linvention-du-stethoscope?mode=desktop
https://www.britannica.com/biography/Johannes-Muller
https://books.google.fr/books?id=MIm4BAAAQBAJ&pg=PA7&lpg=PA7&dq=johannes+peter+m%C3%BCller+cancer+microscope&source=bl&ots=iy4JPo0fij&sig=ACfU3U0ZYWPErry1IkzjDrFOUBpzQSjPYQ&hl=fr&sa=X&ved=2ahUKEwj1orr64bnmAhXEYMAKHQK-BoIQ6AEwEXoECAoQAQ#v=onepage&q=johannes%20peter%20m%C3%BCller%20cancer%20microscope&f=false
https://baillement.com/lettres/mueller_bio.html
https://www.medarus.org/Medecins/MedecinsTextes/virchow_rudolf.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5665122/
https://www.humanite.fr/avec-les-rayons-x-et-la-radiologie-rontgen-bouscule-le-monde-588964
https://www.bibnum.education.fr/sites/default/files/RONTGEN-ANALYSE.pdf
https://culturesciences.chimie.ens.fr/content/le-radium-d%C3%A9couverte-utilisation-et-danger
https://www.bibnum.education.fr/physique/radioactivit%C3%A9/sur-les-radiations-invisibles-%C3%A9mises-par-les-corps-phosphorescents
https://musee.curie.fr/decouvrir/documentation/histoire-radiotherapie
https://www.larousse.fr/encyclopedie/divers/radioth%C3%A9rapie/85354
https://books.google.fr/books?id=LteAUrJQyfEC&pg=PA8&lpg=PA8&dq=Katsusaburo+Yamagiwa+Koichi+Itchikawa+cancer&source=bl&ots=RMZjNGX3Mv&sig=ACfU3U0zlWu3cuEFR8fW_wgpZHcYd2grag&hl=fr&sa=X&ved=2ahUKEwjJ4evJ4bzmAhUHxYUKHaIFAZYQ6AEwEXoECAkQAQ#v=onepage&q=Katsusaburo%20Yamagiwa%20Koichi%20Itchikawa%20cancer&f=false
https://jcs.biologists.org/content/121/Supplement_1/1.full
https://www.medecinesciences.org/en/articles/medsci/full_html/2014/07/medsci2014306-7p679/medsci2014306-7p679.html
https://curie.fr/dossier-pedagogique/cancer-quand-la-cellule-semballe
https://www.allodocteurs.fr/se-soigner/histoire-de-la-medecine/paul-ehrlich-le-pere-de-la-chimiotherapie_16952.html
https://www.biusante.parisdescartes.fr/sfhm/hsm/HSMx2014x048x004/HSMx2014x048x004x0469.pdf
http://www.arcagy.org/infocancer/traitement-du-cancer/traitements-systemiques/chimiotherapie/les-medicaments/les-principes-generaux.html/
https://dtp.cancer.gov/timeline/noflash/milestones/M4_Nixon.htm
https://www.emro.who.int/fr/noncommunicable-diseases/annual-events/journee-mondiale-cancer-4-fevrier.html
https://www.santepubliquefrance.fr/maladies-et-traumatismes/cancers